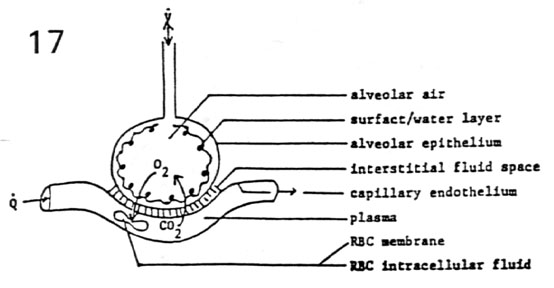
- Thickening of alveolar capillary membrane
- Low hemoglobin
- Decreased alveolar surface area
- Decreased pulmonary capillary bed
- V/Q mismatch
Print version of Knowledge bytes used in this lesson.
Close the window to return to the lesson after printing.
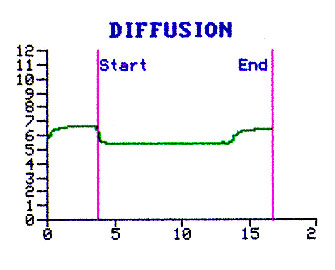
Spirometry
Objectives
To detect presence or absence of obstruction in Spirometry.
- To judge severity of obstruction.
- To be able to detect significant change following bronchodilator administration?
- To identify patterns of flow volume loops in locating the site of obstruction.
Criteria for Obstruction:
Criteria for judging severity of Obstruction:
Criteria for significant change Never use % change of FEV1/FVC
You evaluate for a significant change in the following
If there is a significant change in 2 of 3 it is a significant bronchodilator response.
If 1 of 3 shows a significant change it is borderline response.
If none of them show a significant change no response.
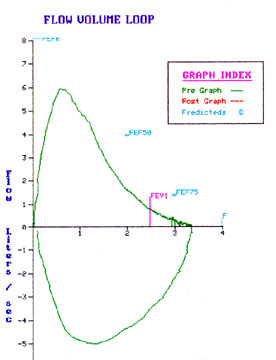
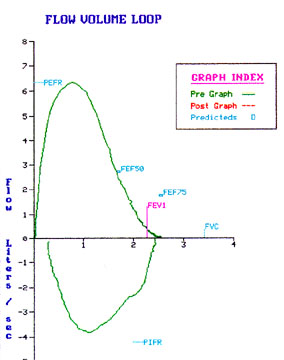
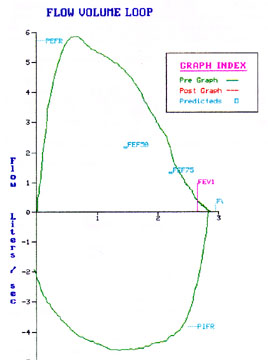
Flow volume loop pattern
The flow volume loop has a typical obstructive pattern as seen in patients with COPD.
Lung Volumes
Objectives
To detect restrictive defect.
- Understand the difference between restrictive defect and restrictive disease.
- Judge severity of restriction.
- To be able to detect significant change following therapy.
- To identify pattern of flow volume loop.
Criteria for restriction:
Caution: Do not make definitive comment about restriction from Vital capacity. If a patient has marked hyperinflation, Vital capacity can be reduced. If the flow rates are increased along with reduced Vital capacity one can surmise there may be restriction. It is always a good idea not to commit yourself about restriction until TLC is available.
Severity of restriction: When the predicted % of TLC is
Criteria for a significant change:
Lung volumes should increase at least by 10% of predicted value to consider it as a significant change. The 2 standard deviation of repetitive performance of lung volumes is 10%. Hence one cannot consider a change as significant unless it is over 10% of predicted value.
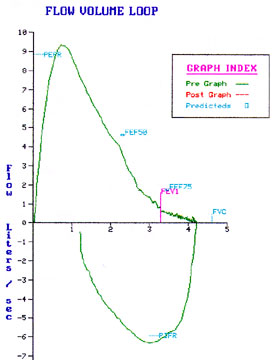
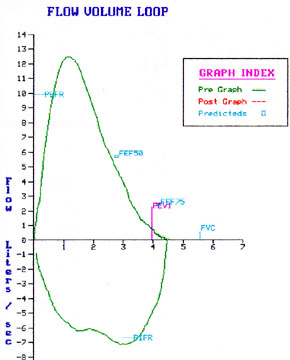
Restrictive pattern in the flow volume loop:
Caution: When the Vital capacity is small computer changes the dimensions of graphic display and you may not appreciate the characteristics.
Restrictive defect: is a PFT interpretation term. Anytime the TLC is less than 80% of predicted we interpret the patient as having a restrictive defect. There are many conditions with normal lungs and reduced TLC e.g. Pregnancy.
Restrictive disease: refers to diseased lungs with reduced TLC e.g. Diffuse interstitial fibrosis.
Restrictive defect:
Lung diseases
Lung resection
Abdominal distension
Chest wall problems
Pleural disease
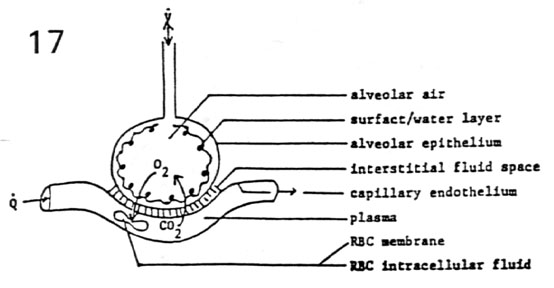
Diffusion
Objectives
To detect diffusion defect.
- Judge severity of defect.
- Variables causing diffusion defect.
- To be able to detect reason for diffusion defect?
- To validate appropriate performance of test.
Diffusion defect is considered present when the % predicted diffusion is less than 75%.
The 2 std deviation for normal range is 25%.
Severity of diffusion defect:
Variables causing diffusion defect:
|
 |
The primary object of performing the test is to identify alveolar capillary membrane thickness. We have to find ways to make corrections for other variables.
| In performing DLCO we ask the patient to inhale an air mixture containing
Carbon monoxide and Helium. Helium is added to obtain the alveolar surface area for that
breath (single breath TLC). Patient is expected to hold the breath for 10 seconds and
exhale. Technician collects the terminal portion of exhalation (alveolar air) and measures
the carbon monoxide concentration. A complex formula is then used to calculate DLCO and VA
BTPS. Obtain the current Hemoglobin to make the necessary correction. In evaluating the graph note the depth of inhalation, duration of breath holding and the timing of collection of alveolar air. |
 |
Flow volume loop Objectives
 |
|
 |
 |
 |
 |
 |
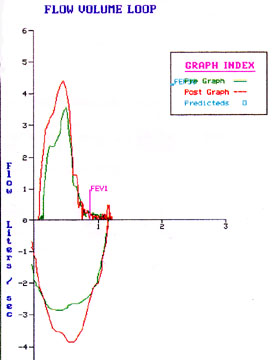
Bronchodilator response
Objectives
What is a significant change for a given test?
There are two ways of looking for a significant change.
I was taught to use the last criteria. 2 standard deviation for repetitive performance of these tests is 10%. Hence it stands to reason that we can consider a change as significant only when it is over 10% of predicted change. Most of the Pulmonologists will use a combination first two criteria to assess a significant change.
Some patients can deflate following relief of obstruction and can increase Inspiratory flow rates. Look at the flow volume loop for these changes.
What criteria do you use to classify a response as significant, borderline and no response?
Indices we are looking at are:
Caution: Be careful with FEF25-75. If the FVC volume changes you cannot use the change in FEF25-75. The mid portion of FVC (FEF25-75) can shift to left (steep portion) or right (flat portion) if the FVC volume changes.
What is the significance of assessing a bronchodilator response?
Caution: Lack of response does not rule out Asthma. Patient could have been already on maximal bronchodilator therapy or may be refractory at the time of bronchodilator administration.
In practice we give bronchodilators to all patients who are obstructed irrespective of the results from PFT study. Hence the exercise in judging the significance of bronchodilator response is more an intellectual curiosity than of practical value.