Utility of Imaging Modalities in Neurological disorders
Objectives:
- List various neuro imaging modalities.
- List unique characteristics of each imaging modality.
- List common indications and contraindications for each imaging modality.
- Differentiate between blood, air, fat, CSF and bone in each imaging modality.
- Learn terms used in describing structures and lesions in each imaging modality.
Topics that will be covered:
Brain
- Skull x-ray
- CT scan
- MRI scan
- Ultrasound
- Cerebral angiogram
- CT angiogram (non-invasive)
- MR angiogram (non-invasive)
- Digital subtraction angiogram (invasive)
Spine
- Plain x-ray of spine
- CT spine
- MRI spine CT myelography
- Bone scan

Skull x-Ray PA view
Skull x-rays are rarely used in the modern days for evaluation of neurological problems. CT and MRI have replaced plain x-rays.
It is primarily useful to evaluate skull bones, base of skull and sinuses. It used to be the initial imaging study in head trauma.
CT has replaced skull x-rays as the initial imaging study for trauma and to evaluate skull and sinuses.
Skull x-rays have not been useful to evaluate brain and intracranial contents. MR is the current imaging modality for that purpose.

Skull x-Ray Lateral view
Skull x-rays can detect bony abnormalities.
- Fractures
- Metastatic lesions
- Multiple myeloma
- Paget's disease
- Alteration in pituitary fossa
- Sinus problems
CT is superior to plain films in evaluating skull bones and sinuses.
MR is the optimal study for evaluating intracranial structures brain, meninges, ventricles etc.
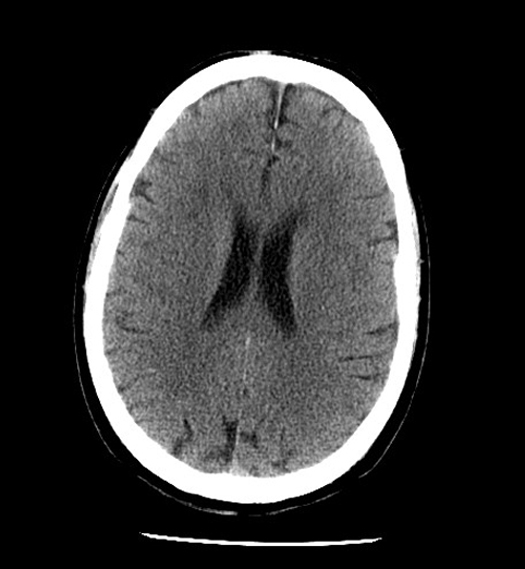
CT scan of the Brain
Advantages:
- CT scan is the imaging modality of choice in patients with history of trauma and acute neurological emergencies where a quick management decision is necessary.
- CT is the study of choice in detecting acute blood than MRI.
- CT is the initial study for stroke if fibrinolytic therapy is a consideration to make sure that it is not a hemorrhagic infarct.
- CT scan can be completed in less than 30 seconds, if necessary in critically ill patients.
- Less of a problem with motion as the study can be completed rapidly.
- CT provides detailed evaluation of bone. Bone is dense with highest CT attenuation value (+1000 H.U.). H.U. stands for Hounsfield unit, named after Godfrey N. Hounsfield, the inventor of computer tomography (CT scan). CT can provide detailed information about the bone which is useful in cases of trauma and in differentiating malignant bony tumors from benign tumors.
- No risk to patients with magnetic medical devices, such as pacemaker, aneurysmal clips, intraocular metallic foreign body.
- It is less expensive compared to MRI.
- CT is useful for routine follow up to evaluate hydrocephalus. Follow-up requires studies of the brain to evaluate hydrocephalus following placement of ventricular shunt catheter.
- Intravenous contrast CT study serves two purposes: 1) to visualize the vessels (CTA), and 2) to detect whether the blood brain barrier is broken. Lesions enhance when the blood brain barrier is broken.
Disadvantages:
- Radiation is a disadvantage to the study. Hence, it is not the preferred study in children. When there are situations where repeated evaluations are necessary, this becomes a problem.
- Iodinated contrast is used and has the potential for allergic reactions.

MRI Scan of the Brain
Advantages:
- MRI is the imaging modality of choice for any patient (adults or children) with neurological deficit, while CT is the choice for head trauma.
- MRI is a more sensitive tool to evaluate sub-acute to chronic hemorrhage.
- Diffusion wtd MRI is more sensitive in detecting early stroke and cerebral abscess.
- MRI is more sensitive in the assessment of structural etiology for seizures.
- MRI has a greater range of soft tissue contrast and depicts anatomy in detail and is much superior to CT. Hence, it is optimal for evaluation of any patient suspected of brain pathology.
- Bone shows up as hypointense (dark) area. Thus, bony architecture is better evaluated by CT imaging. CT is better for evaluating bones.
- MRI does not use ionizing radiation. Hence, it is the preferred study in children and adults.
- Gadolinium is the contrast agent used in MR and causes far less allergic reactions.
Disadvantages:
- MRI brain study is a lengthy procedure compared to CT (average time 30 minutes). Patients may have trouble staying still and supine for that length of time.
- MRI cannot be used in patients with magnetic implanted devices like pacemakers, cochlear implants or with metallic fragments in eye, or aneurysmal clips.
- In patients with compromised renal function, Gadolinium can cause nephrogenic systemic fibrosis.
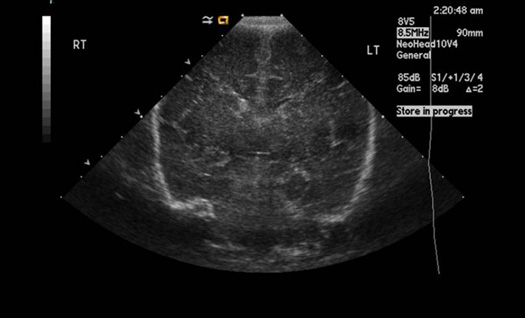
Ultrasound (US)
US does not penetrate bone easily. Hence, it's not useful with adult head.
It is useful in children where fontanels are not closed.
US of normal neonatal child is shown on left.
No radiation is involved with US and hence, ideal for use in neonatal skull.
Children have unique neurological problems like congenital abnormalities, brain tumors and hydrocephalus where US is useful.
It is a non-invasive study with no complications and can be done by the bedside.
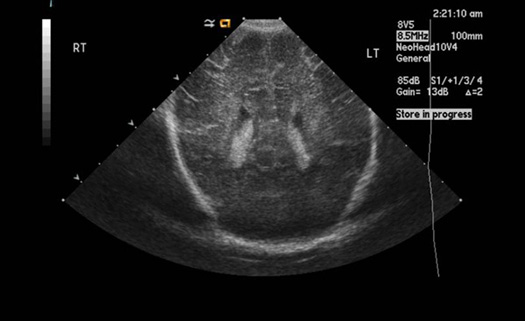
Ultrasound (US)
Normal neonatal child
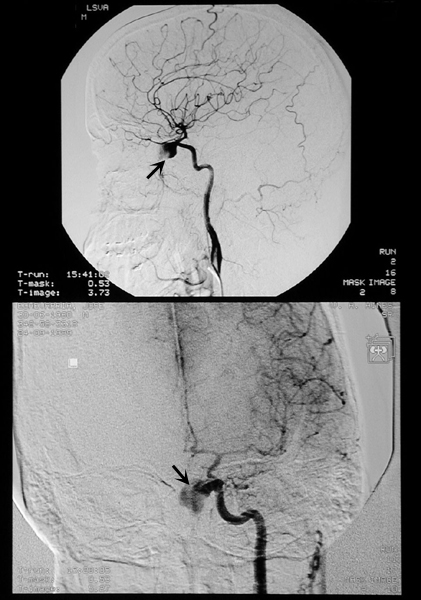
Digital Subtraction Contrast Angiogram
An angiogram uses iodinated contrast agent to make the blood vessels visible under x-ray.
It requires arterial puncture (femoral artery commonly used) followed by advancement of guide wire. Then a catheter is advanced over guide wire to desired location of the vessel. Contrast is injected and pictures are taken rapidly before the dye dissipates.
Advantages:
- Procedure of choice to evaluate extra cranial and intracranial vessels.
- More precise evaluation of intracranial aneurysm, arteriovenous malformation, arterial occlusion, particularly when interventional treatment is contemplated.
- To diagnose vasculitis.
Disadvantages:
- Radiation
- Contrast allergy
- Arterial puncture
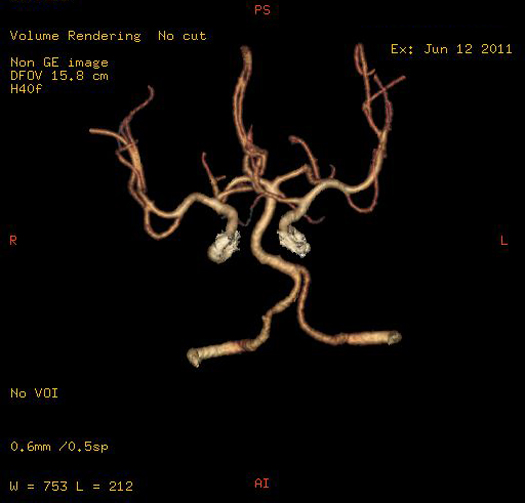
CT angiogram (CTA)
In CTA contrast material is injected into a vein to produce detailed images of blood vessels.
CT imaging produces multiple images and the computer joins them together in multidimensional views.
Advantages:
- Procedure of choice to evaluate extra/intracranial vessels.
- More precise evaluation of intracranial aneurysms, arteriovenous malformations and arterial occlusion, particularly when interventional treatment is contemplated.
- Procedure of choice to evaluate vasculitis and to evaluate smaller vessels.
Disadvantages:
- Radiation
- Contrast allergy
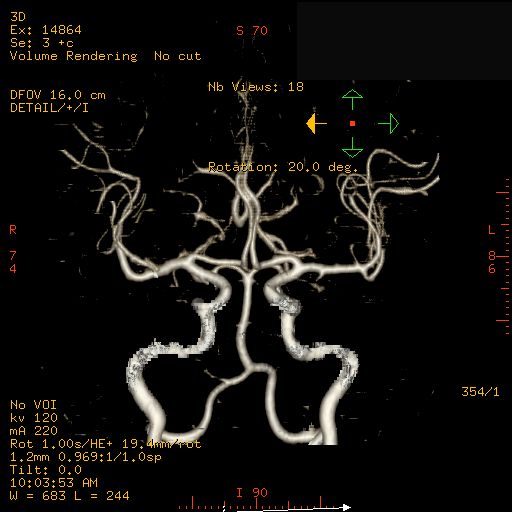
MR Angiogram
MR angiogram, unlike CT angiogram and invasive digital subtraction angiogram, does not display the lumen of the vessel, but rather the blood flowing through the vessel.
Contrast is not required for the study, which is an advantage.
Circle of Willis is shown in the adjacent box.
MR angiogram is less sensitive in detecting smaller intracranial vessels when compared to CT angiogram.
MR angiogram is a screening test.

Plain film of lumbar spine
X-rays are widely available to rule out gross fractures, vertebral pathology or spinal instability.
Normal lateral lumbar spine shown on left.
Plain films of spine can detect
- Fractures
- Displacement
- Alignment problems
- Metastatic lesions
- Osteoporosis
- Vertebral collapse
- Vertebral infections.
Plain films of spine are usually the starting imaging study for back pain either based on clinical examination or bone scan.
CT scan is done if further evaluation of bony lesions is necessary.
MR is done for evaluation of spinal cord, dura, nerve roots and disc.
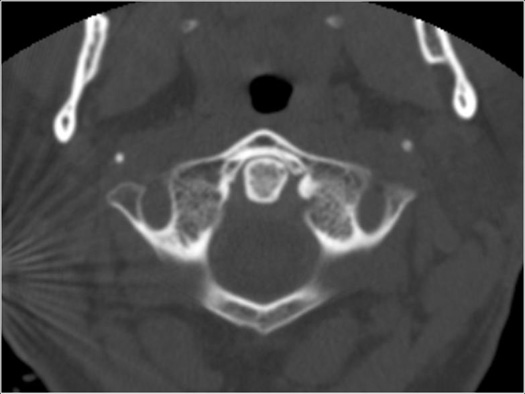
CT cervical spine
Normal CT cervical spine shown on left.
CT scans are commonly used to identify vertebral bone pathology.
CT scans are axial images.
- Bone: Hyperdense appears white
- CSF: Hypodense appears dark
- Cord: Hypodense appears gray
- Disc: Hypodense appears gray
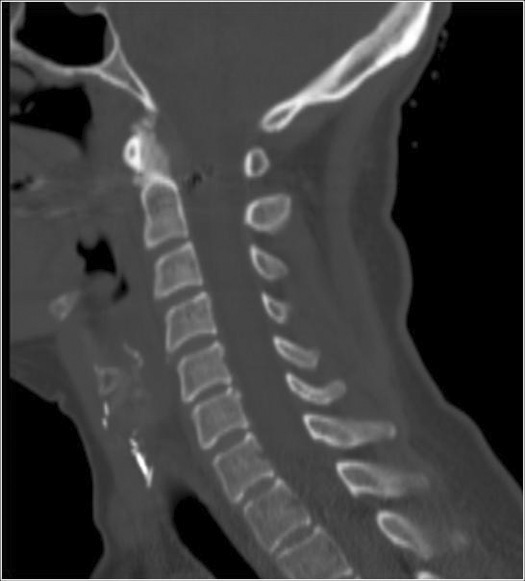
Reconstructed CT cervical spine
CT studies are axial images. Images can be reconstructed for better assessment of the extent of the lesion and relationship to other structures.
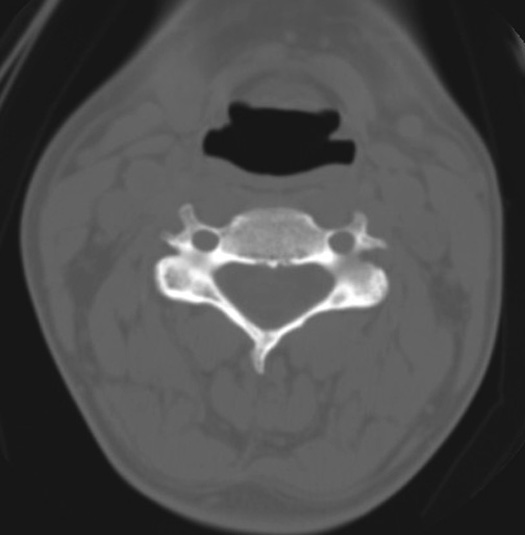
Normal CT cervical spine
CT scans are commonly used to identify vertebral bone pathology.
- Bone: Hyperdense appears white
- CSF: Hypodense appears dark
- Cord: Hypodense appears gray
- Disc: Hypodense appears gray

MR spine
Optimal procedure for evaluating spinal cord and spine.
MR provides exquisite detailed anatomy and alterations from any pathology.
Various pulse sequences are utilized in MR to study the problem.
T1 wtd image and Gadolinium contrast studies should always be looked as a pair of images. When there is enhancement with contrast it indicates that the blood brain barrier is broken.
MR Spine T1 wtd image is seen on left.
CSF is dark in T1 wtd image.

MR spine T2 wtd image
- MR is more accurate and allows visualization of the spinal cord and nerve root compression.
- MR is the best imaging technique to evaluate patients with spinal cord compression. MR images of the entire spinal cord are done so other sub clinical lesions are not missed particularly when cord compression is suspected from metastasis.
Bone: Hypointense and appears gray
CSF: Hyperintense and appears bright
Cord and nerve roots: Hypointense and appears dark
Disc: Hypointense and appears gray
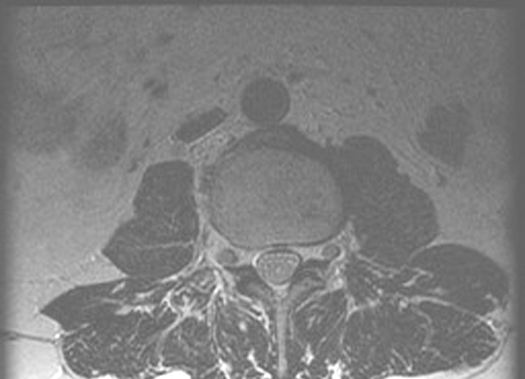
Normal Axial MR Scan
This scan is taken below the level of the cord. The nerve roots (black) are seen floating in the CSF (white).
Axial scans are useful to study disc herniation, compression on cord and neural foramen.

Normal Bone Scan
Whole body nuclear bone scan, a screening test to rule out metastasis to the entire skeleton. Abnormal sites in bone scan will need further evaluation by CT scan.
Normal bone scan in a patient with breast carcinoma. The study was done to rule out metastasis.
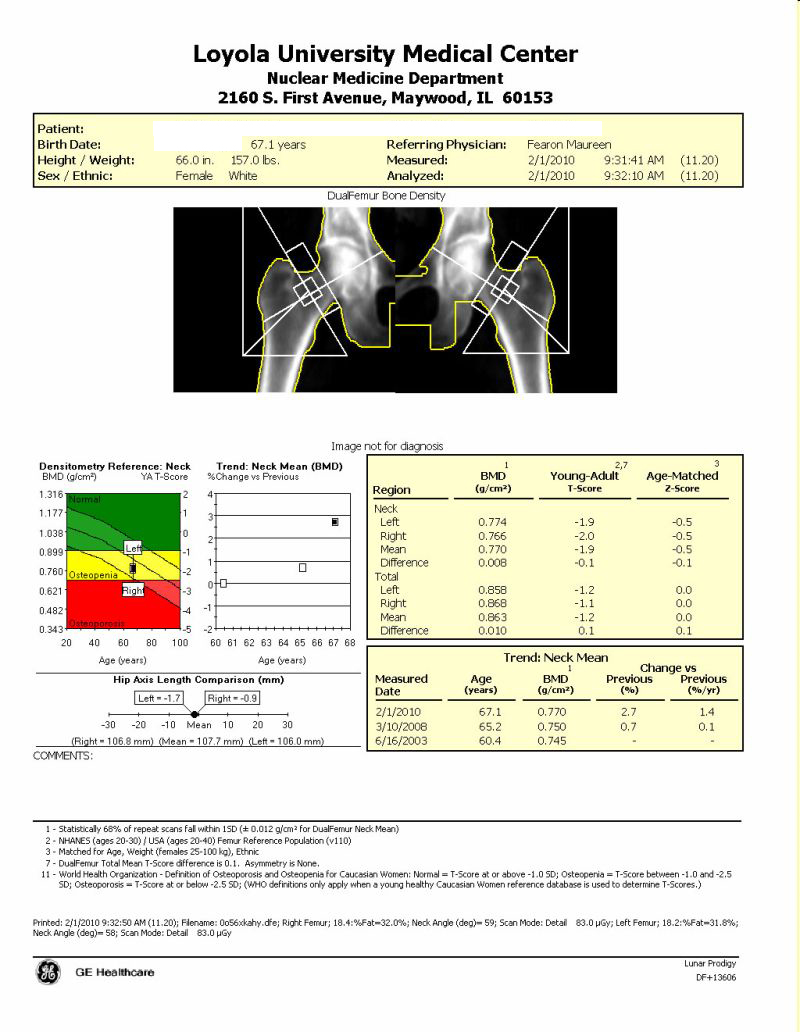
BMD test is the best way to identify patients with osteoporosis, determine risk for fractures and measure response to osteoporosis treatment. A DXA test measures bone mineral density and compares it to that of an established norm or standard to give a score.
Common indications for imaging study of the brain:
Clinical symptoms:
- Headache, nausea, vomiting
- Change in mental status (acute or chronic)
- Seizures
- Head trauma
Clinical signs:
- Focal neurological deficit
- Signs of increased intracranial pressure
- Signs and symptoms suggestive of:
- acute stroke
- subarachnoid hemorrhage
- brain tumor
- meningitis/abscess
- demyelinating disease (e.g., multiple sclerosis)
Common indications for MRI spine:
Clinical symptoms:
- Back pain, neck pain
- Weakness of arms, legs
Clinical signs:
- Upper extremity/lower extremity weakness
- Focal neurological deficit
- Congenital disorders
- Demyelinating disease
- Patients suspected of
- spinal trauma
- spinal infection
- spinal cord tumor
- spinal cord compression
Identification of blood, air, fat, CSF and bone in imaging studies
Blood |
Air |
Fat |
CSF |
Bone |
|
| Plain films | White | Dark | Dark | White | |
| CT | Hyperdense / Bright | Hypodense / Dark | Hypodense / Dark | Hypodense / Dark | Hyperdense / Bright |
Hounsfield Units Applies to CT |
50-80 H.U. |
-1000 H.U. | -10-100 H.U. | 0 H.U. | +1000 H.U. |
| MR T1 wtd image | Hypointense / Dark | Dark | Hyperintense / Bright | Hypointense / Dark | Hypointense / Dark |
| MR T2 wtd image | Dark | Hyperintense / Bright | Hyperintense / Bright | Hypointense / Dark | |
| Ultrasound | Anechoic (flowing blood) | Does not transmit | Hyperechoic / Does not transmit | Anechoic | Hyperechoic / Does not transmit |
Be familiar with the terms used in CT, MR and US and plain films. Each tissue is recognized by its unique characteristics. In addition with CT you can obtain Hounsfield units that specifically indicate which tissue we are dealing with.
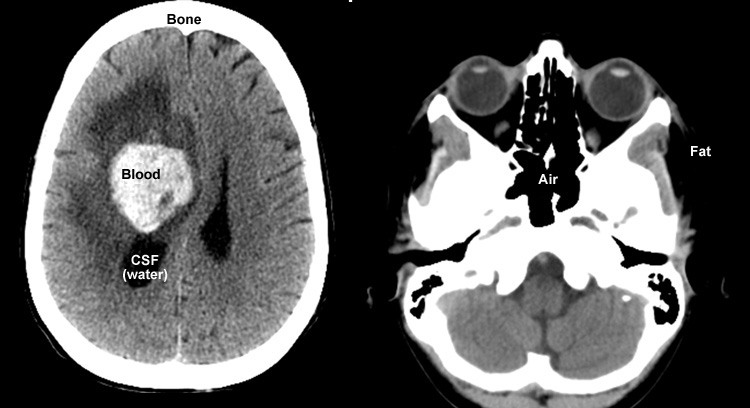
CT Head
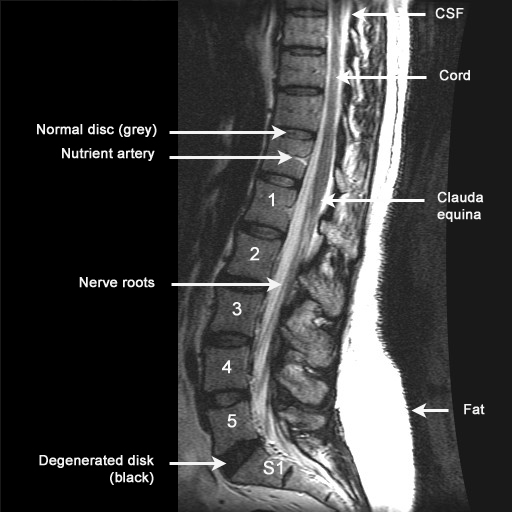
MR spine T2 wtd. image
Bone: Hypointense / Gray
Disc: Hypointense / Gray
CSF: Hyperintense / Bright
Spinal cord and nerve roots: Hypointense / Dark
Fat: Hyperintense / Bright