
Physicians are one part of a large network of providers for each patient.
Introduction / Textbooks / Equipment / Attendance / Evaluation Policy
PCM is a 3 year course designed for Loyola medical students to develop the skills needed to become balanced, competent, patient-centered physicians with life-long career satisfaction.
Patient Centered Medicine is based on the idea that the patient is at the center of the health care team, and each member of the team has an important role to play in promoting the patient’s health and happiness.
The health care team is only a small part of the patient’s life.

Physicians are one part of a large network of providers for each patient.
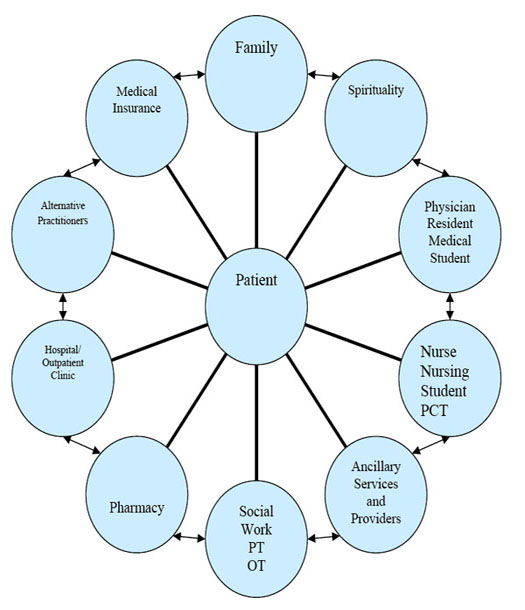
Each member of the health care team must partner with all of the other members of the team as well as the patient for the desired outcome of health and happiness.
From the very first day of medical school, medical students are an important part of that health care team. PCM will help students define their own roles as learners and providers on this team. Therefore, this course has the expectation that each student will work to his or her capacity at all times.
PCM requires the integration and synthesis of work learned in this and other courses as well as experiences outside of the classroom. The expectation is that every student has the goal of becoming the best physician (s)he can become, and will actively work toward that goal in all PCM and SSOM activities. Students are not passive learners in PCM and are expected to take responsibility for their own education within the framework presented. This model is very different than the undergraduate model of didactic lecture and student regurgitation of knowledge.
Learning in PCM is based on lectures, panel discussions and significant hands-on small group and experiential activities. These activities may include mentor programs, shadowing programs, simulated patients- both virtual and actors, real patient encounters, reflection papers and discussions, reading books and journal articles, small group discussions and practice of skills learned, working with ancillary health providers, and many skills workshops.
Topics will range from taking a basic medical history, and performing a physical exam to understanding medical errors, patient safety issues, reading EKG’s and X-rays, understanding medical ethics and many more.
Overall, By the END of PCM 1, students are expected to:
| SSOM Objective ID | Course Objective ID | Course Objective | Assessment Method(s) |
| 2.1, 3.2, 3.3, 3.5 | PCM1-1 | Demonstrate proficiency in medical communication, to include taking a patient centered, complete medical history and educating and counseling patients and families accross the broad range of socioeconomic and cultural backgrounds | Standardized patients, small group observation and feedback, facilitator formative and summative feedback |
| 2.1 | PCM1-2 | Demonstrate proficiency in performing a basic physical examination | SP, OSCE |
| 2.1, 3.4 | PCM1-3 | Construct a comprehensive written patient history | Facilitator informal evaluation, multiple choice individual assessment |
| 5.5 | PCM1-4 | Evaluate bioethical issues according to prescribed methodology | multiple choice examination |
| 3.5 | PCM1-5 | Interpret challenging interpersonal situations and apply effective communication skills | small group facilitator evaluation (summative and formative) |
| 4.1 | PCM1-6 | Employ self assessment and reflection techniques with regards to participation and performance in multiple settings | small group facilitator evaluation (summative and formative) |
| 1.6, 1.7 | PCM1-7 | Apply statistical methods to biomedical questions | multiple choice examination, problem sets |
| 2.6 | PCM1-8 | Apply evidence based medicine to questions of patient care including screening and risk factor analysis | multiple choice examination |
| 2.6 | PCM1-9 | Apply techniques of health promotion and disease prevention in patient interactions | Standardized patients, small group observation and feedback, facilitatory formative and summative feedback |
| 8.1 | PCM1-10 | Utilize and foster skills necessary to support life-long career satisfaction | facilitator feedback |
| 5.1-5.6 | PCM 1-11 | Demonstrate behaviors appropriate to the profession in all course activities including collaborative interprofessional practice | Standardized patients, small group observation and feedback, facilitator formative and summative feedback, multiple choice examination |
| 6.1-6.4 | PCM1-12 | Evaluate the effects of healthcare delivery systems and laws on individuals and populations | Multiple choice examination, group essay, small group observation and feedback |
| 1.6 | PCM1-13 | Apply principles of screening and behavior change counseling to patients with harmful or risky behaviors | Multiple choice examination, group essay, small group observation and feedback |
| 3.1, 3.3 | PCM1-14 | Develop skills involved in oral presentation of medical cases | facilitator informal evaluation |
| 6.3 | PCM1-15 | Describe the major factors that contribute towards a culture of safety within healthcare systems | multiple choice examination, small group observation |
REQUIRED:
SUGGESTED:
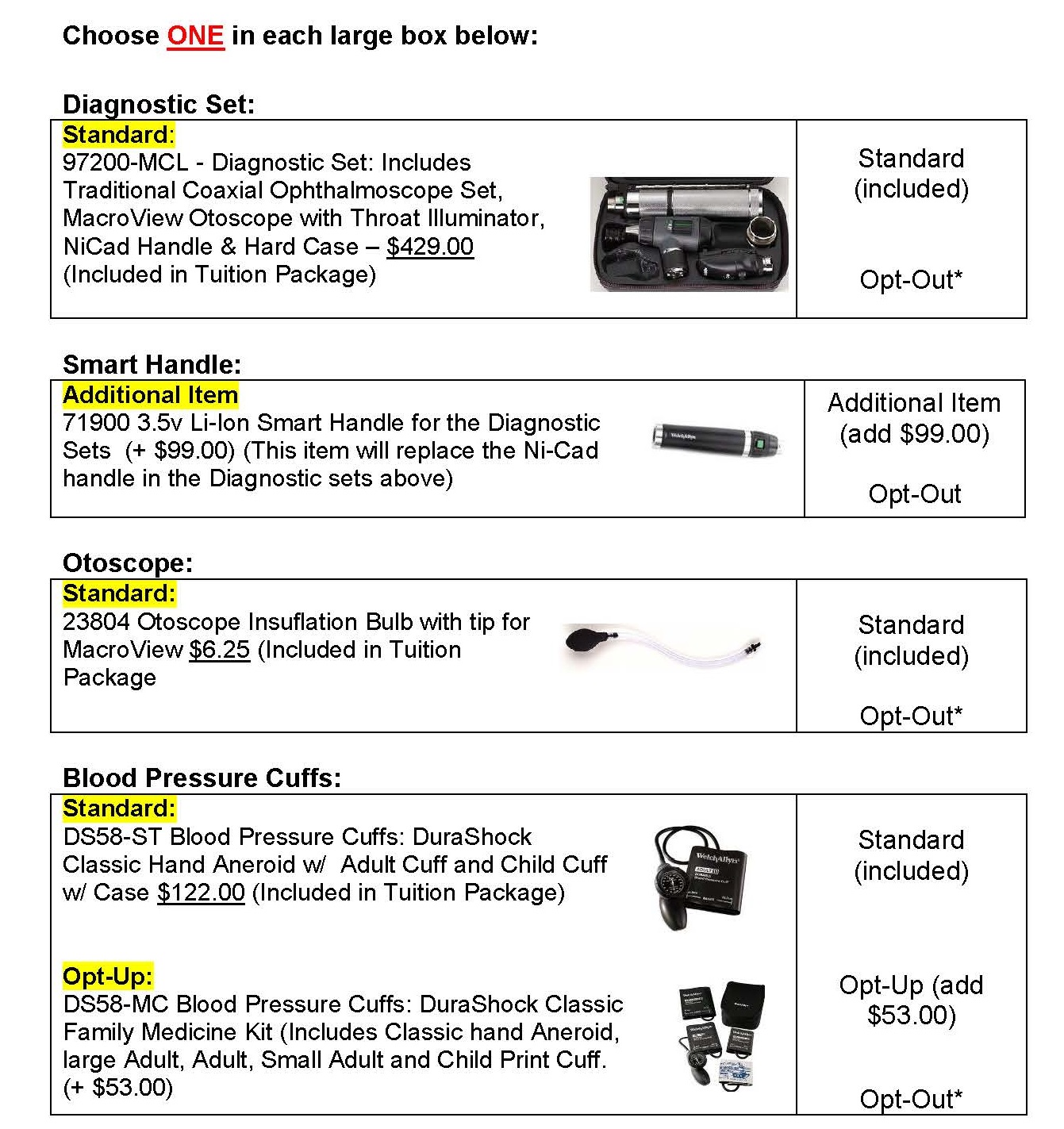
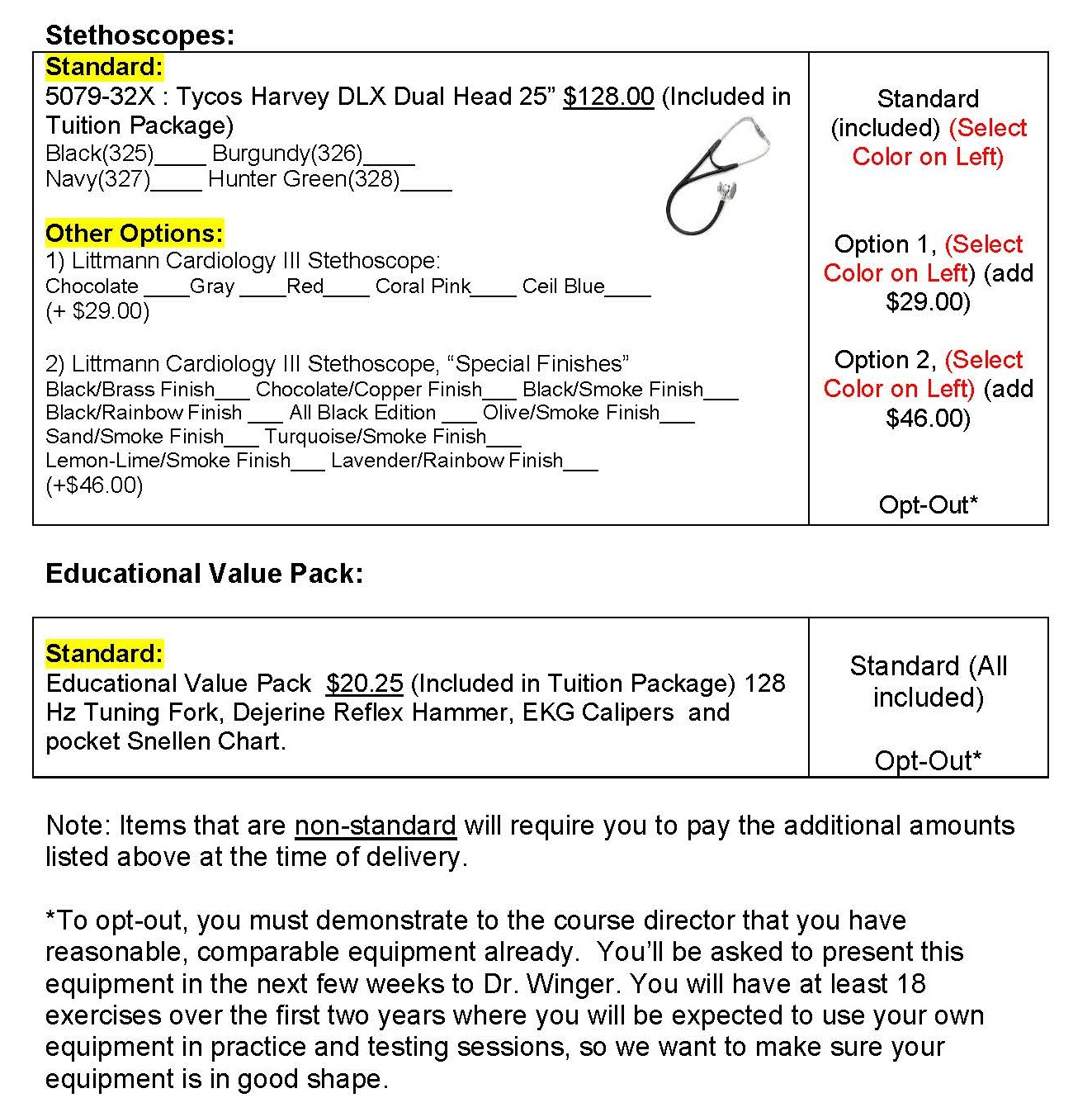
Diagnostic equipment and stethoscope will be provided by the PCM-1 course. Further information will be given during orientation week.
NOTE: You will be using your equipment with your Clinical Skills Preceptors, mentors, in your standardized patient experiences, your small groups, your volunteer experiences, in the summer immersion trips and for the rest of your life as a practicing physician.
Every component of PCM 1 is considered important for the professional development of first year medical students. Therefore, the expectation is that students will attend all components of PCM 1. However, it is understood that emergencies arise and students may need to miss an activity.
Each of the 6 components of PCM 1 has a very specific attendance policy:
You may be expected to make up work missed for emergencies. Failure to comply with this attendance policy may result in failure of PCM 1.
For any emergency- please notify the Patient Centered Medicine 1 Medical Education Coordinator- Ms. Diane Stancik at 708-216-8219.
Patient Centered Medicine 1 is a "Pass/Fail" course. To pass, each student must pass all 6 components of the course.
All evaluation in PCM 1 is based on the following 3 categories:
"Meets Expectations” means that the student is doing well, and is meeting the benchmark set for a solid, average medical student.
"Meets Expectations with Concerns” means that the student is meeting the benchmark, but at a minimum level, and there are concerns that this student may need some extra assistance or work in a particular area to eventually pass the course.
“Does Not Meet Expectations” is a red flag that the student is not meeting the minimum level set for competency in this area. This indicates the student is currently failing PCM-1.
Expectations of PCM
1 Students
2)
To be prepared, on time, and actively participate in all
PCM activities
3)
To attend all PCM activities, and to sign in only for
her or himself when attendance is taken
4)
To complete all assignments on time, and to the best of
her/his abilities
5)
To not cheat, lie, or falsify information
6)
To dress appropriately, act professionally, and
represent Loyola well at all times
7)
To treat her/his peers, teachers, course administrators,
education specialists, health care professionals, all LUHS and SSOM employees,
patients, all she/he contacts as a medical student, and especially her or
himself with the utmost respect at all times
8)
To collaborate with everyone involved in her/his
education, including her/his peers to learn how a team functions to care for
patients
9)
To ask for help when needed
10)
To be open to the ideas of others and to feedback about
her/his own performance and progress from all sources
11)
To accept that we are all human, and all make mistakes
and to take responsibility for and learn from mistakes
12)
To be patient, flexible, and open to unknown or
unconsidered possibilities
13)
To approach all PCM activities in the spirit of wonder,
inquisitiveness, learning, self-improvement, gratitude and humility
Expectations of PCM
1 Facilitators
The following represents a limited, but not all
inclusive, list of expectations for PCM 1 Facilitators:
1)
To create a safe learning environment within the small
group
2)
To help each student hold him or herself to the
expectations of PCM students
3)
To set standards for and help each student to work to
his or her potential
4)
To role model collaboration and teamwork
5)
To role model the idea of patient centered care in all
PCM activities
6)
To facilitate learning and growth in all small group
members, including her/himself
7)
To be prepared, on time (within reason), and actively
facilitate in the small group
8)
To dress appropriately, act professionally, and
represent Loyola well at all times
9)
To treat her/his peers, other teachers, course
administrators, education specialists, health care professionals, all LUHS and
SSOM employees, patients, all she/he contacts as a teacher, and especially
her/himself with the utmost respect at all times
10)
To ask for help when needed
11)
To be open to the ideas of others and to feedback about
her/his own performance and progress from all sources
12)
To accept that we are all human, and all make mistakes
and to take responsibility for and learn from mistakes
13)
To be patient, flexible, and open to unknown or
unconsidered possibilities
14)
To approach all PCM activities in the spirit of wonder,
inquisitiveness, learning, self-improvement, gratitude and humility
Remediation Policy:
If at any time a student earns a single mark of “Does Not Meet Expectations", (s)he will be considered to be failing that component of the course and will need to remediate that component. If the student fails a final component of the course (i.e., final SP exam, final OSCE, final small group evaluation, etc.), (s)he will fail the course. Per school policy, the student will be given an opportunity to remediate that component after the course has ended. If the student successfully completes this remediation, then the student will earn a grade of P* (Remediated Pass). If the student earns “does not meet expectations” on the second remediation, the student fails the remediation and must repeat the course in its entirety.
PCM1 consists of the following components:
Grading Versus Competency Evaluation
Your performance is evaluated throughout PCM 1 using a “Competency Based System.” This means that a standard has been set which defines what it means to be competent with a skill set.
The competencies for this course are listed in the “General Information” section of the PCM 1 website and are based on the 6 competencies set by the Stritch School of Medicine:
Meeting the level set as competent in each of the 6 competencies above will mean that you will pass the course. A grade of “P++”, (earning a "Pass" in a Pass/Fail course), will appear on your permanent transcript – this is your grade for PCM 1.
However, you are also evaluated in each competency by the levels set above as “Meets Expectations”, “Meets Expectations with Concerns”, and “Not Meeting Expectations.”