Learning Objectives: You should be able to:
- Trace the pathways molecules of oxygen and carbon dioxide
must traverse as pulmonary capillary blood become arterialized.
- Contrast the diffusion constant for any gas versus
diffusing capacity of the lung in mathematical terms of Fick's law of
diffusion.
- Plot as a function of time the change in blood P02
and PCO2 as venous blood flows through the lungs.
- List and explain four different causes of arterial
hypoxemia found in abnormal human pathophysiology.
Rhoades & Tanner Text Readings: Chapter 21, Pages 386-391,
395-398
Diffusion Path
Diffusion Capacity Alveolar
Gas Partial Pressure A-a
Gradient Hypoxemia
MainMenu
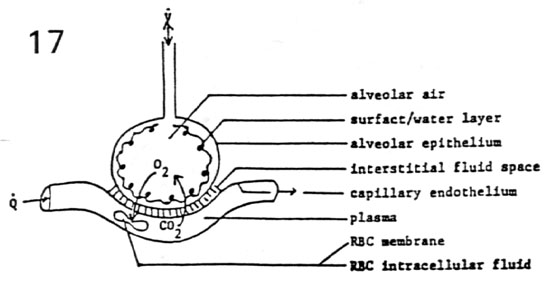
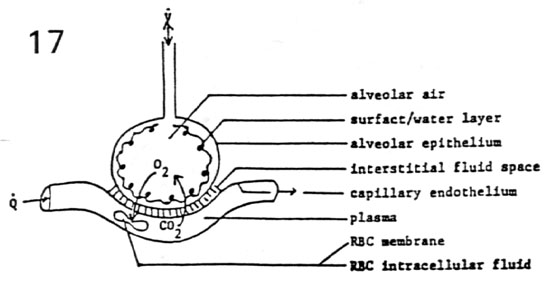
Diffusion Pathway
- Diffusion
- passive diffusion and catalytic action of carbonic
anhydrase
- facilitated diffusion (cytochrome P-450 fixed site O2
and CO carrier)
- Respiratory Membrane and Barriers to Diffusion
Diffusion Path
Diffusion Capacity Alveolar
Gas Partial Pressure A-a
Gradient Hypoxemia
MainMenu
Diffusing Capacity of the Lung
- Gas Fluxes Across a Resistive Barrier
 gas =
gas =  Pgas * (1 / R)
Pgas * (1 / R)
 gas =
gas =  Pgas * G
Pgas * G
- where:
 = diffusive gas flow (mL/min)
= diffusive gas flow (mL/min)
- R = resistance to diffusive gas flow (mm Hg/[mL/min])
- G = conductance to diffusive gas flow ([mL/min]/mm
Hg)
 P
= (PP1gas - PP2gas) pressure gradient (mm Hg)
P
= (PP1gas - PP2gas) pressure gradient (mm Hg)
- PP1 & PP2 = partial pressures of given gas
species on either side of membrane
- Expansion of Fick's Law
 gas =
gas =  Pgas * G
Pgas * G
 gas =
gas =  Pgas * DL gas
Pgas * DL gas
 gas =
gas =  Pgas * (areamem/thicknessmem) * Dgas
Pgas * (areamem/thicknessmem) * Dgas
 gas =
gas =  Pgas * (areamem/thicknessmem) * (sol.gas/
mol. weightgas)
Pgas * (areamem/thicknessmem) * (sol.gas/
mol. weightgas)
- DL gas = diffusing capacity of the lung
to the gas
- Dgas = diffusion constant for the gas
- Factors Favoring High Gas Conductance (DL gas)
- gaseous phase (1/ mol. weightgas)
- low molecular weight of gas
- short diffusion path in gaseous phase
- respiratory membrane phase (areamem/thicknessmem)
- thin membrane (t = 0.2-1.0 µm)
- large gas exchange area (A = 70 m2 = 750
feet2)
- high lipid solubility of gas
- aqueous phase (sol.gas)
- high fluid solubility
- fast reaction rate with hemoglobin
- small pulmonary capillary diameter (8 µm)
- large red blood cell diameter (5-8 µm)
Diffusion Path
Diffusion Capacity Alveolar
Gas Partial Pressure A-a
Gradient Hypoxemia
MainMenu
Alveolar Gas Partial Pressure
1. Dalton's Law of Partial Pressures

- Ptotal = P1 + P2 + P3
for a three-gas mixture
- P3/Ptotal = %P3 present in
total gas mixture
- Ptotal = Patm for dry air (e.g.
atmosphere)
- Ptotal = Patm - PH2O for
100% humidified air (e.g. trachea)
- PH2O = 47 mm Hg at 37°C
- atmospheric %O2 = 20.9%
- atmospheric %CO2 = 0.03%
Physiologic
Region |
PO2
(mm Hg) |
PCO2
(mm Hg) |
| inspired air |
159 |
0.23 |
| trachea |
149 |
0.21 |
| alveolus |
100 |
40 |
| pulmonary vein |
95 |
40 |
| pulmonary artery |
40 |
46 |
- important notes
- pulmonary artery (high pressure) contains deoxygenated
blood (from systemic veins)
- pulmonary vein (low pressure) contains oxygenated blood
(to systemic arteries)
- PAO2 can be computed from the
alveolar gas equation
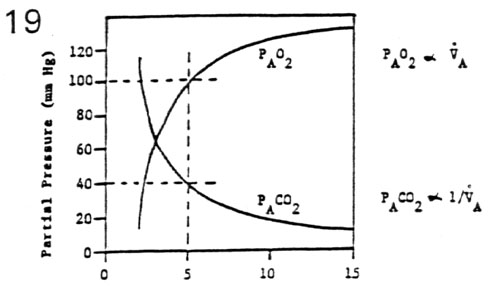
2. Variations in Alveolar Ventilation
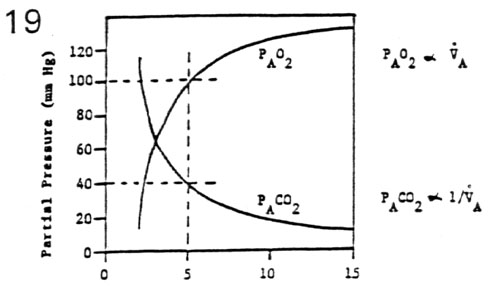
 A = f * (VT - VD) = (10/min) * (0.65 L -
0.15 L) = 5.0 L/min
A = f * (VT - VD) = (10/min) * (0.65 L -
0.15 L) = 5.0 L/min
- mean PAO2

 A and
mean PACO2
A and
mean PACO2  1/
1/  A
A

 A above metabolic demand results in hyperventilation with
A above metabolic demand results in hyperventilation with  PAO2 and
PAO2 and  PACO2
PACO2

 A
below metabolic demand results in hypoventilation with
A
below metabolic demand results in hypoventilation with  PAO2 and
PAO2 and  PACO2
PACO2
- such changes in ventilatory PACO2 are
important for maintaining acid/base balance
Diffusion Path
Diffusion Capacity Alveolar
Gas Partial Pressure A-a
Gradient Hypoxemia
MainMenu
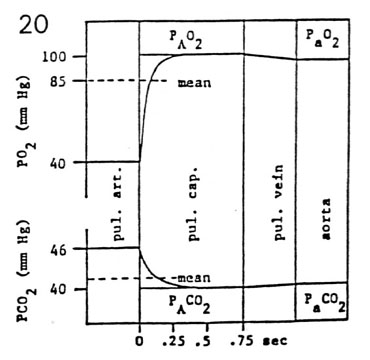
Alveolar-Arterial Gradient
- Red Blood Cell Transit Time
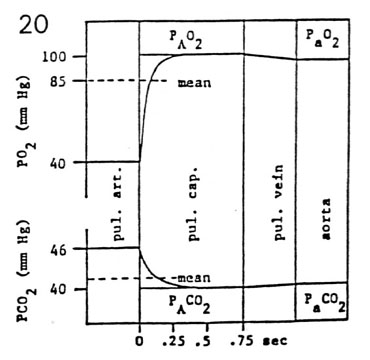
- Ttransit = pulmonary capillary volume /
cardiac output
- Ttransit = (75 mL) * (60 sec/min) / (6000 mL/min)
= 0.75 sec
- normally, gas equilibrations across the
alveolocapillary membrane are complete in 0.25 sec
- the safety factor for gas equilibration is 0.5 sec or
2/3 of the cap length
- abnormal gas equilibrations
 Ttrans (< 0.25 sec) due to
Ttrans (< 0.25 sec) due to  pulmonary capillary volume or
pulmonary capillary volume or  cardiac output
cardiac output
 respiratory membrane conductance (DLgas)
respiratory membrane conductance (DLgas)
- Anatomical and Physiological Shunts
- systemic arterial gas tensions are not exactly matched
to mean alveolar gas values
- PaO2 < PAO2
by
 5 mm
Hg and PACO2 > PACO2 by
5 mm
Hg and PACO2 > PACO2 by  0.5 mm Hg (A-a gradient)
0.5 mm Hg (A-a gradient)
- A-a gradient is attributed shunt flow bypassing the gas
exchange zone
- anatomical shunts: post-pulmonary shunts, bronchial
circulation, ventricular septal defects
- physiological shunts: ventilation/perfusion
inequalities
- clinically, PaO2 > 85 mm Hg are
considered normal
Diffusion Path
Diffusion Capacity Alveolar
Gas Partial Pressure A-a
Gradient Hypoxemia
MainMenu
Arterial Hypoxemia
- Hypoventilation
- problem: � V A � PaO2 and � CaO2 with no
change in A-a gradient
- nervous system defects (CNS, NM junction)
- toxic drug effects (barbiturates, morphine)
- solution: � V A with possible O2 supplementation
- mechanical ventilation
- respiratory stimulants
- Diffusion Impairment
- problem: � DLO2 � PaO2 and � CaO2 with
� A-a gradient
- interstitial fibrosis (� thickness of alveolar
capillary membrane)
- interstitial pneumonia (� thickness of alveolar
cap membrane)
- pulmonary edema with alveolar flooding (� area
gas exchange)
- solution: � PAO2, but beware of oxygen toxicity
- cute 100% O2 (< 2 days) induces � pulmonary
capillary permeability and alveolar edema
- chronic 100% O2 (> 2 days) induces interstitial
fibrosis & � Clung
- Anatomical Shunt
- problem: � venous admixture � PaO2 & �
CaO2 with � A-a gradient
- normal shunts: venous drainage from thebesian &
bronchial circ
- abnormal shunts: atrial or septal defects, patent
ductus arteriosus
- solution: surgical repair of arterial-venous
anastomosis
- oxygen administration will not help (diagnostic
test for shunt)
- PaCO2 may not be raised above normal (40 mm Hg)
- Ventilation/Perfusion Inequality
- problem: � V A/Q � PaO2 and � CaO2
- chronic obstructive pulmonary disease (COPD)
(emphysema, bronchitis)
- pulmonary embolism
- solution: � PAO2 but be aware of induced �
physiologic shunt blood flow
- very low V A/Q ratio alveolar units may become
atelectic
- PaO2 is still improved with oxygen supplementation
Diffusion Path
Diffusion Capacity Alveolar
Gas Partial Pressure A-a
Gradient Hypoxemia
MainMenu