Case Answers:
Answer 1
“VOPS”
- Ventilatory failure
- Oxygenation
- Protection of Airway
- Secretions
A patient having "The Look" is also an indication for mechanical ventilation
Answer 2
- BiPAP decreases the work of breathing which is often excessive due to the presence of auto-PEEP
- In pooled data, the risk of intubation may be reduced from as high as 75% to as low as 25%. This represents a NNT = 2.
- Clinical setting:
- Sleep Apnea
- Pulmonary Edema secondary to CHF
- Neutropenic Patients with Pulmonary Infiltrates
- The use of CPAP/BiPAP in post-extubation respiratory failure has been studied and, while controversial, has not been shown to be beneficial and, in fact, may increase mortality. This reinforces the concept if a patient needs to be intubated NOW, any delay in doing so might be detrimental.
Answer 3
Clearly, many satisfactory options and therefore would use this opportunity to discuss the relative advantages/disadvantages of various modes and ventilator strategies. For a COPD patient, a generally accepted strategy would include a/c mode with modest TV and Rates, PEEP adjusted to approximately 70% of the estimated intrinsic-PEEP (to minimize the work of triggering the ventilator), a modest FiO2 (since VQ mismatch should be easily correctable), and an I:E ratio of 25% or less (to minimize the likelihood of developing significant intrinsic-PEEP).
Answer 4
- With volume-cycled ventilation (assist control and SIMV), minute ventilation is preserved at the expense of increased airway pressures.
- With pressure-cycled ventilation (pressure support and pressure control), airway pressures are maintained at the expense of decreased minute ventilation and hypercapnia.
Answer 5
- Too large – peak pressure alarm
- Too small – patient appears uncomfortable, gasping for breath
- Just right: Normalized vital signs, reduced respiratory effort/apparent work of breathing, adequate pulse oximeter saturation, absence of abdominal paradox, etc
Answer 6
High?
- Inadequate sedation with excessive catecholamine output.
- Agitation in critically ill patient is usually due to pain, anxiety or delirium
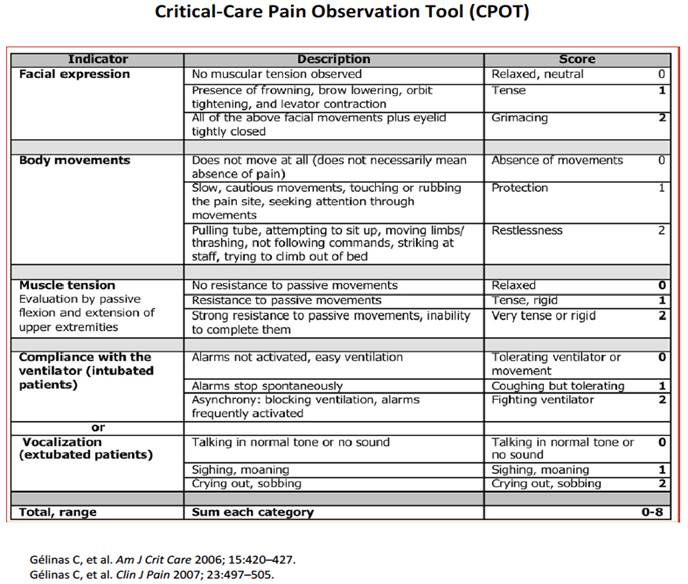
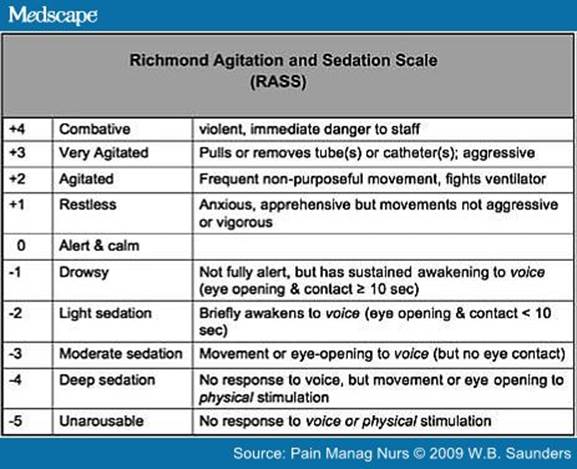
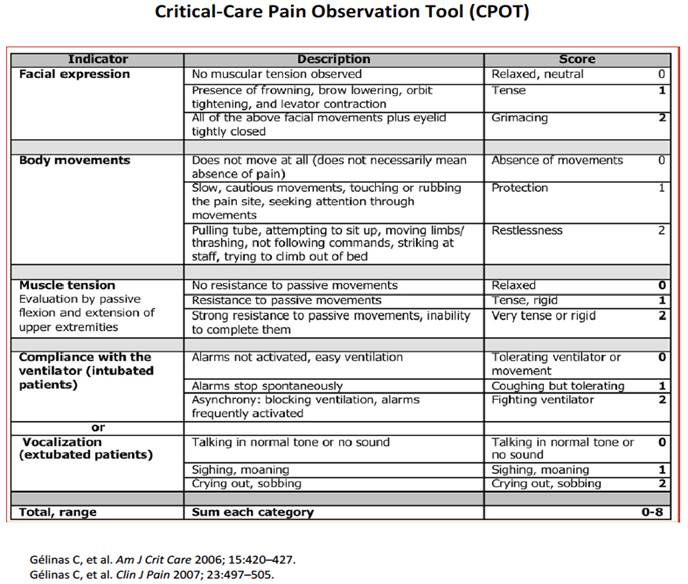
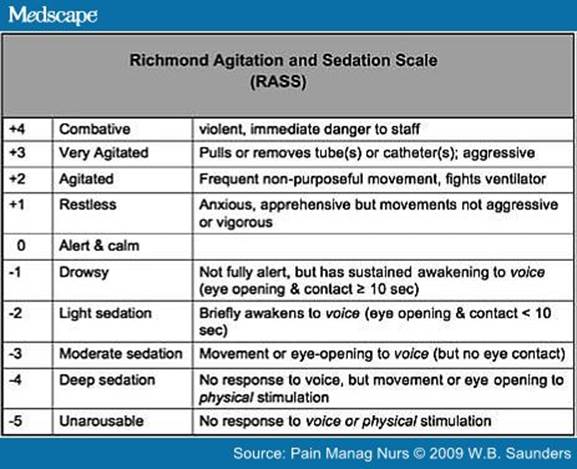
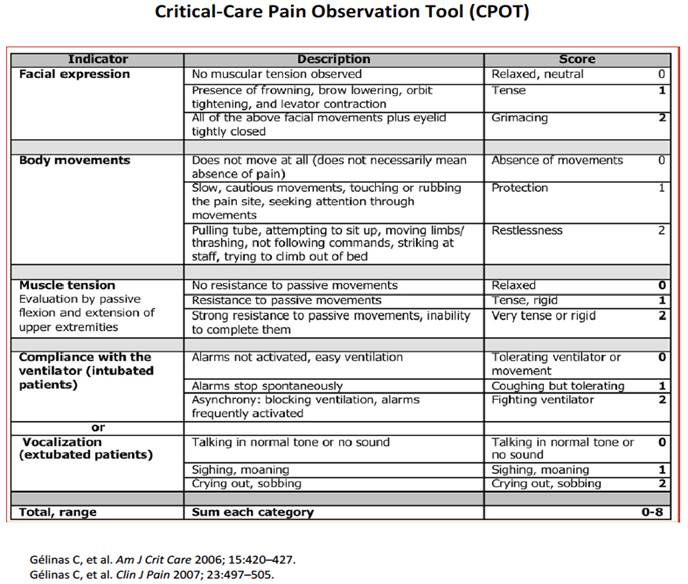
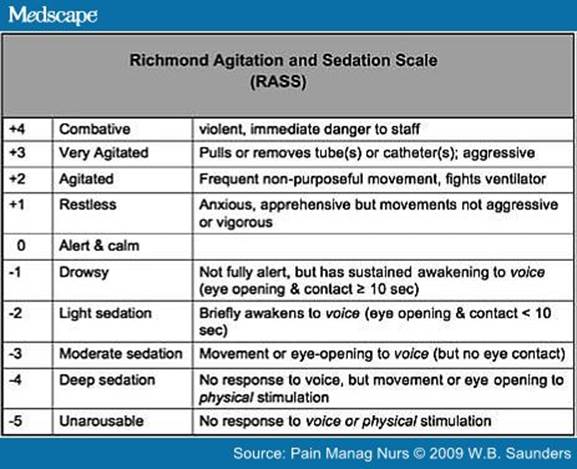
- There are several validated scales that can be used to assess a patient’s pain, agitation and delirium (see attached)
- The CPOT scale is used to assess pain (goal of <3)
- The RASS scale is used to assess agitation (goal of zero to -2)
- The CAM-ICU scale is used to assess delirium (goal of negative)
- Use “analgesia-first” sedation (Treat pain first and then sedate if patient remains agitated.
- Use IV pushes of Fentanyl; start a drip only if necessary to control pain
- Many patients in the ICU will not require a continuous drip for sedation
- Patients should be awake and able to follow commands unless there is a clinical indication for deeper sedation
- If the patient remains agitated despite treating pain, start either propofol or dexmedetomidine (Precedex)
- AVOID benzodiazepines in the ICU unless necessary for EtOH withdrawal -benzodiazepines can lead to delirium and increased ICU stay
Low?
- The change from negative pressure ventilation (i.e., spontaneous breathing) to positive pressure ventilation with resultant increased intrathoracic pressures and decreased venous return +/- the effects of peri-intubation sedatives.
Answer 7
Hypercapnic secondary to increased respiratory system load related to increased airway resistance and intrinsic-PEEP.
Answer 8
V/Q Mismatch which is usually easily corrected.
Answer 9
Compliance = TV / (Pplat - PEEP) = 600/(15 - 5) = 60
Answer 10
The high peak to plateau gradient is most consistent with an increased resistance.
Answer 11
Increased intrinsic-PEEP.
Answer 12
The best ventilator strategy is to decrease the inspiratory time (although this will increase the peak pressure). Decreasing the TV and/or RR may help although in most cases the patient will simply increase their spontaneous TV minimizing the benefit. Continuous bronchodilator therapy, +/- steroids, +/- antibiotics will hopefully reverse the underlying pathology.
Answer 13
Compliance = 600 / (30 - 5) = 24
Answer 14
- Acute in onset
- Severe hypoxemia (P/F ratio < 200)
- Bilateral opacities on Chest X-ray or Chest CT
- Respiratory failure can NOT be fully explained by fluid overload
- An echo should be done if no risk factors for ARDS are present
Answer 15
Hypoxemic (in the acute phase although later, in the proliferative phase, hypercapnic failure may result)
Answer 16
Shunt which is typically relatively refractory to supplemental oxygen.
Answer 17
A number of strategies are employed simultaneously to manage the hypoxemia of ARDS. These include:
- Treat the underlying cause,
- Increasing the FiO2,
- Titrating PEEP,
- Diuresis
- Optimizing the MVpO2:
- Reducing oxygen consumption
- Treat the fever and sepsis,
- Reduce work of breathing through optimizing ventilator settings,
- Sedation
- Neuromuscular blocking agents (Paralytics):
- Monitor the degree of neuromuscular blockade using a peripheral nerve stimulator (or train-of-four monitor)
- A peripheral motor nerve is electrically simulated with four sequential stimuli over a 2 second period
- The paralytic dose is titrated such that only 1-2 visible muscle twitches occur in response to each train-of-four
- Augmenting oxygen delivery
- Blood transfusion
- Use of pharmacologic agents to increase cardiac output.
- Prone positioning
- Consideration of ECMO in rare circumstances (i.e., H1N1 associated ARDS)
Answer 18
- Would focus on the RSBI (rapid shallow breathing index, f/Vt, < 100) and NIF. Various strategies have been used for weaning including intermittent T-Piece trials versus gradual reductions in pressure support or IMV. IMV trials appear to be the LEAST effective means of weaning. TPiece trials and/or Pressure Support trials both have data supporting their use in weaning.
- Loyola has a weaning protocol in place that includes the ABCDE bundle
- Implementation of this bundle has been shown to shorten the duration of mechanical ventilation, ICU and hospital length of stay
- ABCDE bundle involves:
- Daily awakening trials for ventilated patients
- Spontaneous breathing trials
- Coordinated effort between the nurse and respiratory therapy to perform the spontaneous breathing trial when the patient is awake enough
- Delirium assessment and management using CAM-ICU
- Early mobilization and ambulation (Exercise) of critically ill patients
- If the patient is awake enough and has an acceptable RSBI, the patient can be started on a spontaneous breathing trial without getting approval by a physician.
- If the patient does well after a 30-minute spontaneous breathing trial, the RN or respiratory therapist is to notify the physician that patient looks OK to extubate (needs a physician order to do so).