Screening Mammography
Overview:
Glandular tissue and cancerous lesions appear white on a mammogram, whereas fat appears black. In young women, with dense glandular breast tissue, it is very difficult to distinguish cancer from normal glandular tissue. However, as women age, there is a fatty infiltration of the breast, which appears dark on imaging, therefore making it easier to identify cancerous lesions. Mammogram abnormalities include masses, calcifications, asymmetry and architectural distortion. However, these findings must be taken in context of age, since many lesions in younger women (i.e. less than 40) are not cancerous. The most specific mammographic feature of malignancy is a speculated focal mass. In addition, there is a high correlation between a high density mass lesion and malignancy. Clustered microcalcifications measuring between 0.1 to 1 mm in diameter and numbering more than 4 to 5 per cubic cm are seen in 60% of cancers detected by mammography. Linear branching microcalcifications have a higher predictive value for malignancy than do granular microcalcifications, especially for high grade DCIS. It is important to keep in mind that calcifications that are not suspicious for malignancy include vascular and skin calcifications, rim like calcifications, large coarse calcifications and smooth round or oval calcifications.
Objectives
- For early detection of breast cancer
- Sensitivity of the procedure
- Specificity of the procedure
- Yearly for women over the age of 50
- For high risk patients
- Family history of breast cancer - Cancer in first degree mother's side relatives (mother, sister, daughter)
- Prior cancer breast
- Survival advantage of early detection
- Annual cost for population screening
- Number of potential subjects
- Cost per procedure
- Morbidity and harm to patients by investigations with non-specific lesions
- Number of people benefited versus number harmed
How does mammogram differ with age?
In young women the breast is often extremely dense. Glandular tissue and cancer are dense (white) in a mammogram. Hence it is difficult to distinguish cancer from normal dense glandular tissue in young women.
As women age, there is fatty infiltration of the breast associated with atrophy of glandular tissue. Fat is lucent (dark) in mammogram and hence, a cancer is better identified.
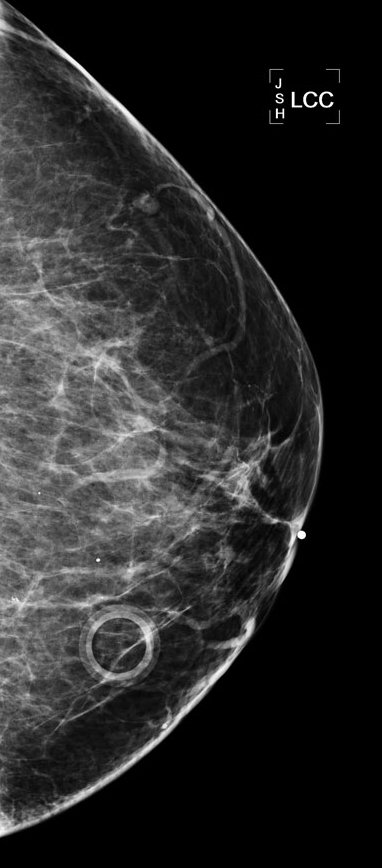 |
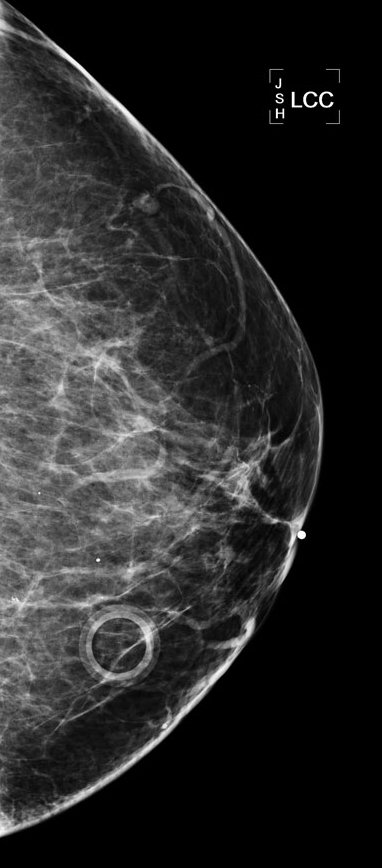
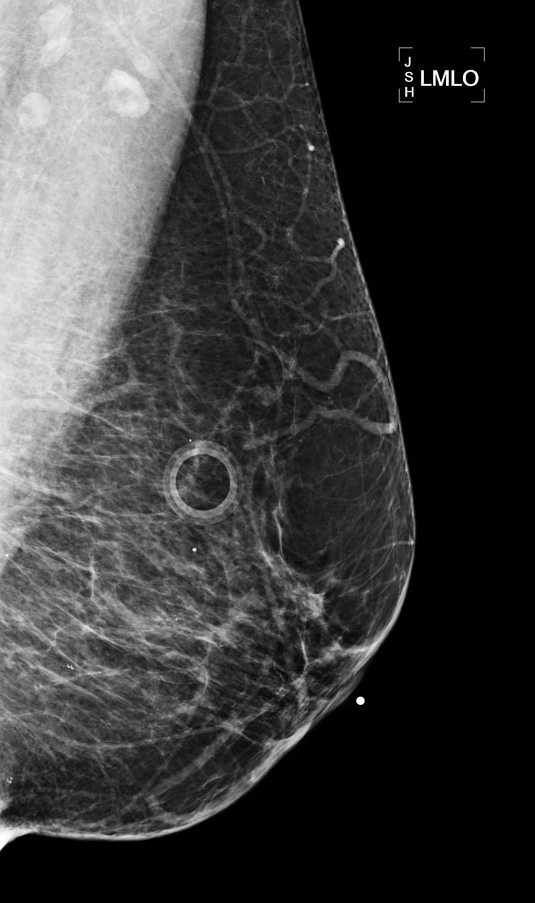
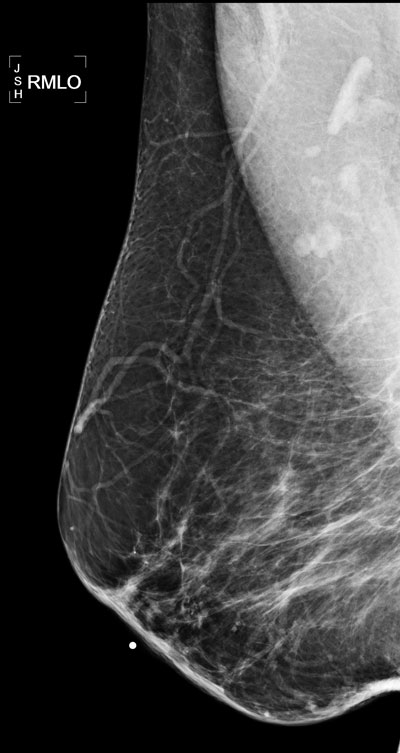
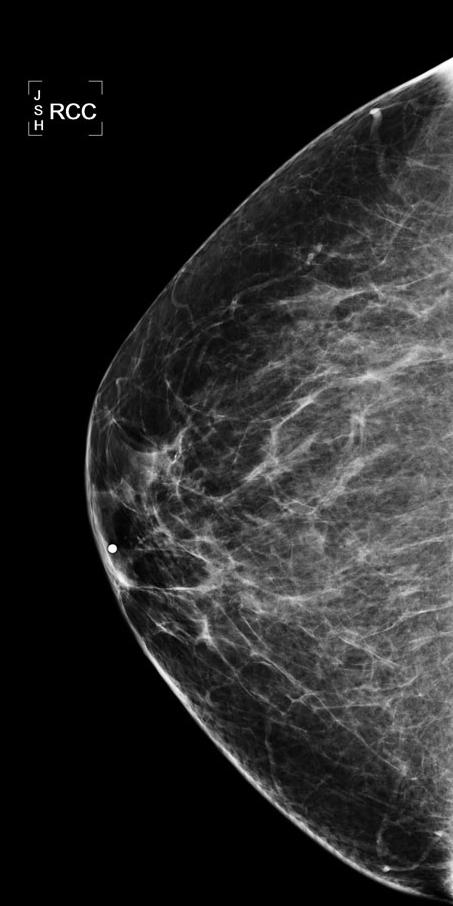
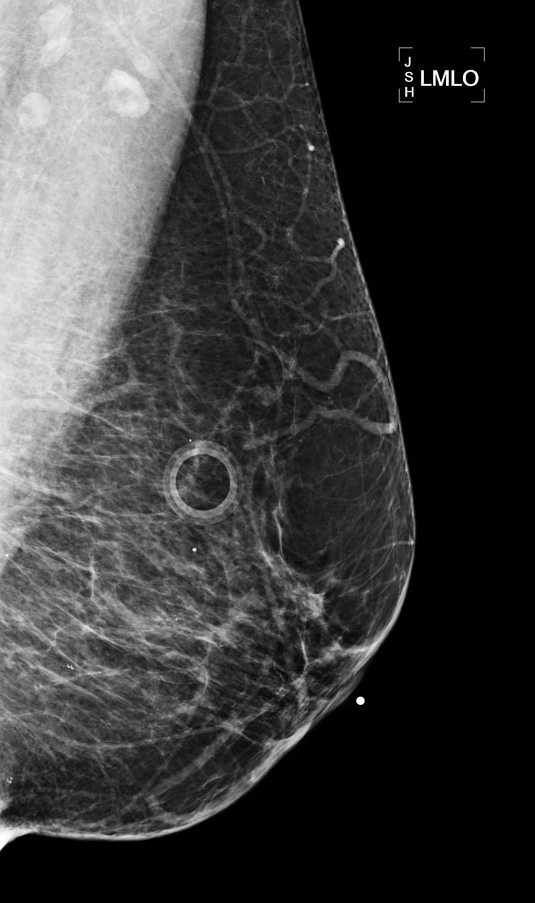
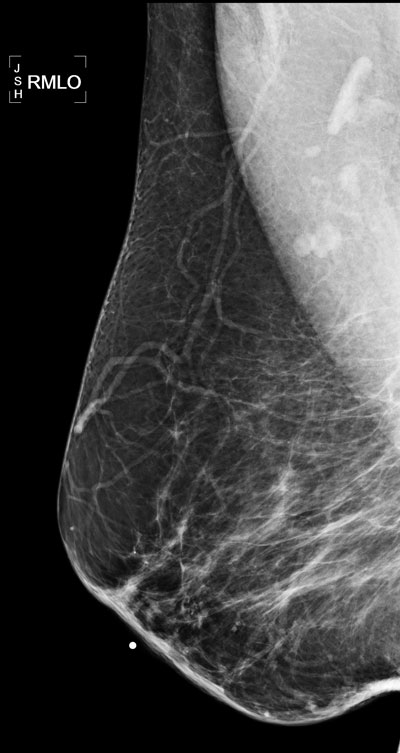
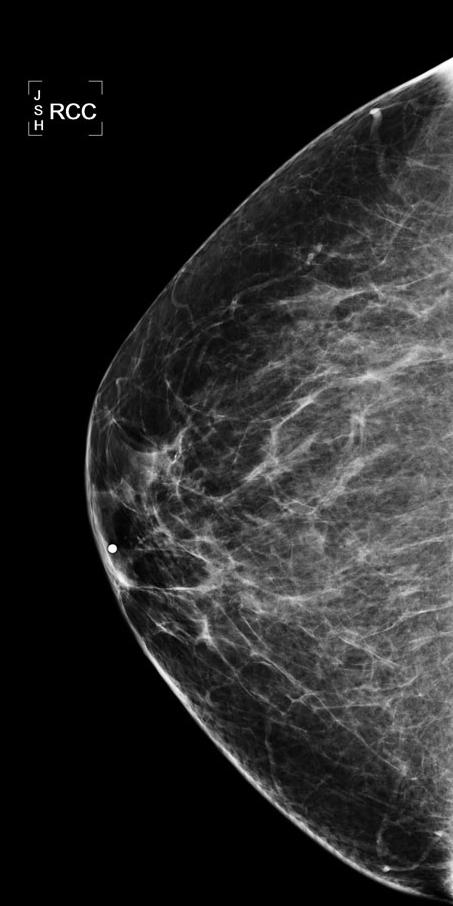
The density of the breasts in this mammogram is consistent with the patients age seen by the fact that most of the dense tissue seen in younger people has been replaced by fat which appears black on the mammogram.
There are a few scattered calcifications widely spread throughout image, but no cluster of calcifications so not very suspicious.
There is a skin marker in image one and two. The marker is placed around skin lesion to ensure that it is not mistaken for breast lesion.
You can also see few lymph nodes in the second image in axilla. Small nodes are normal just like nodes in inguinal region.
|
 |
 |
 |
|
At what age should you start the screening mammography for detection of breast cancer? How frequently it should be done?
Various recommendations are made by different organizations. The generally accepted recommendation is a mammogram each year starting at age 40. This is recommended by the American Cancer Society and the American College of Radiology in addition to many other organizations.
What is the incidence of breast cancer corrected for age?
- Under 20: rare
- Under 30: less than 2% of total cases
- Risk gradually increases after age 40
- Incidence of 300 cases per 100,000 in 8th decade
After which age does the risk of developing breast cancer steadily increase in women?
After the age of 40, a woman's risk of developing breast cancer steadily increases.
Who is at high risk for cancer breast? What risk factors are associated with an increased chance of developing breast cancer?
Risk factors for breast cancer include:
- Gender: less than 1% of incidence occurs in males
- Age: risk increases in women after age 40
- History of cancer in one breast: risk increases 3-4 times
- Family history of breast cancer: 2-3 fold increase risk if first degree relatives had breast cancer
- Non invasive carcinoma (ductal or lobular carcinoma in situ)
- Minor
- Early menarche
- Late menopause
- Nulliparity
- Late first full-term pregnancy
- Low dose radiation
- In Japan there is higher risk for breast cancer in surviving women exposed to radiation from the atomic bomb (only if they were exposed to high doses).
Estimate the accuracy (sensitivity and specificity) of mammography as a screening test.
The sensitivity and specificity values are for women aged 50-70:
- Sensitivity (the ability to detect disease, when disease is present) is 75-94%.
- Sensitivity is lower among women who are less than 50 years old, have denser breasts, or are taking hormone replacement therapy.
- Specificity (the likelihood that a mammogram will correctly indicate that cancer is not present) is 83-98%.
- Specificity is increased with shorter screening intervals and availability of prior mammograms.
What is the false positive rate of mammography?
Given a specificity of 83-98%, false positives occur 2-17% of the time.
What conditions give rise to false positive suspicion for cancer breast?
Several benign breast conditions can produce a spiculated density, which may be indistinguishable on mammography from carcinoma.
Spiculated mass density has been encountered in:
- Post-biopsy scarring
- Traumatic fat necrosis
- Breast abscess
- Sclerosing adenosis
- Radial scar
Also, it may be difficult to distinguish benign from malignant calcifications.
Case 1
A 25 y/o woman who has a strong family history of breast cancer comes to your office inquiring about screening mammography at her age. What would you tell her?
A. Screening mammograms should be done once a year.
B. Screening mammograms should be done once every two years.
C. Screening mammograms are not recommended at this age.
Answer C
- A screening mammogram can be conducted starting ten years before the age of the mother's breast cancer, but not earlier than 25 y/o.
- Screening for detection of early cancer is not indicated for women below 40 years of age.
- The incidence of cancer is extremely low in this age group.
- The breast tissue is dense and recognition of cancer is difficult with mammography.
- Sensitivity is lower among women who are younger than 50 (51 percent to 83 percent) and older than 70. Such values are also lower in women having denser breasts or women on hormone replacement therapy.
Let us now evaluate the evidence and controversy with regards to screening mammography.
What are some potential disadvantages for screening mammography?
- Low specificity
- Cumulative risk of a false-positive result after 10 mammograms is roughly 49%.
- 80-90% of abnormal screening mammograms or CBEs are false positives.
- False positive results can lead to undue stress, discomfort and additional medical expenses.
- Concern for potential over diagnosis of DCIS
- Some studies show that DCIS is being diagnosed more often now. Consequently, some patients may be undergoing major procedures such as masectomy or lumpectomy and radiation for lesions that might not require such aggressive intervention.
- Radiation induced breast cancer
- Estimates of up to 8 potential deaths in a population of 100,000 women screened for 10 years starting at age 40 have been cited ( National Academy of Sciences). However, this is low compared to the number of screening carcinomas found in 100,000 women.
What potential harms can occur from screening for breast cancer with mammography?
- The large majority of abnormal screening mammograms are false-positives.
- These may require invasive follow-up procedures such as unnecessary breast biopsies to resolve diagnosis, which can result in anxiety, inconvenience and additional medical expenses.
Is there a potential risk for radiation-induced breast cancer in women who receive annual mammograms?
- The risk estimate provided by the Biological Effects of Ionizing Radiation report estimated that annual mammography of 100,000 women for 10 consecutive years beginning at age 40 would result in up to 8 radiation-induced breast cancer deaths.
- This risk is negligible compared to the benefits from screening mammography!
- The probability of developing breast cancer between the ages of 40-49 is 1.5%; thus screening mammography would detect 1,500 cases of breast cancer in this age group.
What factors contribute to the annual cost of performing screening mammograms for women as indicated?
- Number of women over the age of 40
- Average cost for screening mammogram
- Annual cost
Screening mammography certainly detects early cancer. What evidence do we have to show that screening mammography and early detection of cancer prolongs life? What is the survival advantage of early detection of breast cancer?
- Widespread use of mammography, alone or with a CBE performed by a trained health-care provider, can reduce overall mortality from breast cancer.
- Since the 1970s, scientific studies have demonstrated that regular screening mammograms among women aged 50-69 years, can reduce mortality from breast cancer by 30%.
- Evidence is not as conclusive for women aged 40-49 years and > 70 years.
Screening mammogram reveals a suspicious lesion for cancer in left breast. No mass is palpable. How would you proceed?
- Core biopsy with stereotactic or ultrasound guidance (preferable method); or
- Radiologist performs needle localization procedure:
- Breast is compressed with a holder that has coordinates on the sides, and mammogram is obtained.
- A thin needle is placed in the lesion through coordinates.
- A blue dye is injected at the site.
- A thin hooked wire is passed to the lesion where it gets fixed.
- The needle is withdrawn leaving the wire in place.
- Surgeon removes the tissue around the wire tip.
- The biopsy specimen is x-rayed to make sure that the suspicious lesion was removed.
Case 2
A 35 year woman with a strong family history of breast cancer comes to the clinic inquiring about screening. She has no other risk factors other than family history. What would you tell this patient regarding the current recommendations for breast cancer screening?
Answer:
- There is no need for mammography at this time.
- Instruct the patient to do self-exams.
- It is recommended that self breast exams are done once a month in the shower; however, the USPSTF concludes that there is not sufficient evidence to support or oppose this teaching.
Discussion of current recommendations:
- The USPSTF recommends biennial screening mammography for women aged 50 to 74
years.
- The USPSTF recommends screening mammography, with or without clinical breast examination (CBE), every 1-2 years for women aged 40 and older (B recommendation)
- The decision to start regular, biennial (every 2 years) screening mammography before the age of 50 years should be an individual one and take patient context into account, including the patient's values regarding specific benefits and harms.
- There is insufficient evidence to recommend for or against CBE alone for diagnosing breast cancer (USPSTF).
- There is insufficient evidence to recommend for or against teaching or performing routine self breast exam.
Case 3
CHIEF COMPLAINT: “I want a mammogram.”
A 40 year old female presents to clinic asking for a mammogram. She is a healthy, active woman with a medical history significant only for hypothyroidism and cholecystectomy at age 35. She is a homemaker and mother of 2 children. She has never smoked cigarettes, and drinks one glass of wine with dinner each night. She states that her mother died of breast cancer at age 60, and a previous family doctor had advised her to start screening for breast cancer with mammograms at age 40. The patient's obstetric/gynecologic history includes the following information: menarche age 12, menses occurs regularly every 28 days and lasts for 5 days. She is gravida 2, para 2.
PHYSICAL EXAM: The breasts are examined with the patient in sitting and supine positions. The breasts are large, round and symmetrical. The contour of each is smooth with no evidence of dimpling, retraction or edema. The nipples and areola are symmetrical, pink-tan and show no eczema or inversion. Palpation of both breasts and axilla reveals no abnormalities.
Answer: This patient should have a screening mammogram.