Deep vein thrombosis (DVT)
What are the predisposing factors for DVT?
- Diminished blood flow, or stasis, occurs with immobility or during bed rest, during surgery, and in patients with heart failure or chronic venous insufficiency.
- Endothelial vessel damage occurs during surgery, burns, and as a result of trauma.
- Hypercoagulable states can be acquired or inherited.
- Many situations can lead to acquired hypercoagulable states, including cancer, pregnancy, certain medications such as oral contraceptives, smoking, and other diseases such as systemic lupus erythematosus.
What are the symptoms and signs of DVT? When would you suspect DVT?
- A DVT should be suspected in any patient who presents with a risk factor as well as unilateral leg swelling, pain, warmth, and/or erythema.
- This standard presentation is infrequent.
- The clinical exam is an inadequate method for diagnosis of DVT.
- DVTs are often clinically insidious and are only diagnosed after emboli have traversed to the lung.
What are the useful imaging studies available to investigate deep vein thrombosis? What is the utility of each?
- Contrast venography
- Gold standard
- Better in identifying calf vein thrombosis
- Increased risk of phlebitis and contrast related problems
- Invasive and painful
- Compressive duplex ultrasonography
- Noninvasive
- Poor visualization of iliac, and pelvic veins
- Requires skilled operator
- Can be repeated serially to monitor suspected DVT
- Poor sensitivity in identifying calf vein thrombi
- Positive predictive value of serial compressive ultrasonography is generally higher than that of classic IPG.
What is the sensitivity and specificity of each in detecting deep vein thrombosis?
- Contrast venography -- This test is the current gold standard, and is considered nearly 100% sensitive and specific in the diagnosis of DVT. However, it is a painful and invasive test and requires the administration of contrast material.
- Compressive duplex ultrasonography -- Duplex ultrasound is a reliable noninvasive method of detecting DVTs. This involves both compression and doppler ultrasound and is 90-100% sensitive and 80-100% specific for proximal DVT.
What are the radiological criteria for deep vein thrombosis in duplex ultrasound exam?
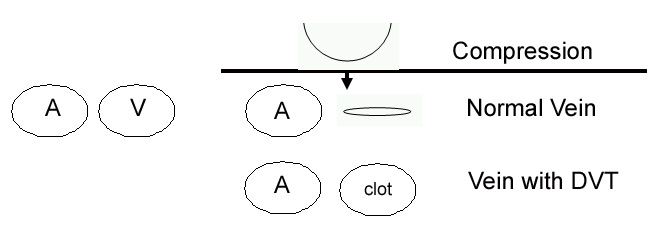
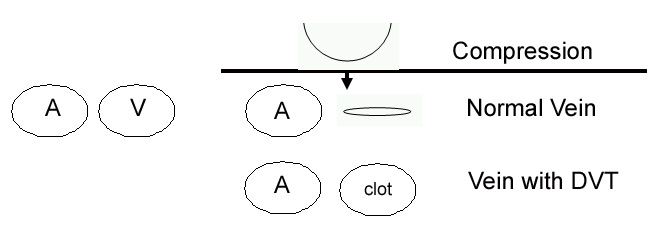
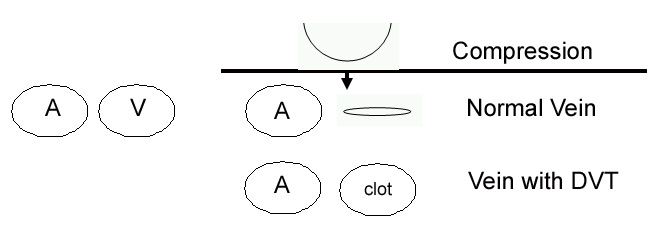
- A venous compression ultrasound views the femoral artery and vein in two-dimension.
- Pressure is applied to the thigh, which should induce compression of a patent vein.
- If a thrombus is present, pressure cannot compress the vein and a DVT is suspected.
- On the doppler ultrasound, decreased or absent spontaneous venous blood flow is assessed to identify DVTs.
What is the role of venogram in the evaluation of deep vein thrombosis?
- Venogram even though is the gold standard, is a painful and invasive test and requires the administration of contrast material. Hence, it is performed only when absolutely essential.
- Venogram is in the algorithm of suspected calf vein thrombosis as other modalities have poor sensitivity in detecting it.
- However, it is rarely necessary, because a distal thrombus has a low risk of embolization.
- These patients are closely followed.
What is the optimal sequence of imaging procedures in the investigation of deep vein thrombosis?
- First-line testing for DVTs involves the noninvasive method of ultrasound using doppler.
- Although they are not as sensitive or specific as contrast venography, they are rarely contraindicated and are convenient to perform.
- Venography is performed only when other studies are inconclusive and diagnosis is necessary.
A case of deep vein thrombosis:
The patient is a 24 year old female who presented to the ER with complaints of chest pain and difficulty breathing. The pain was in her right upper chest, sharp, sudden, non-radiating, and she had never experienced it before. It occurred while she was at rest. She had not been lifting heavy weights or exercising lately.
- Past medical/surgical history: Appendectomy at the age of 12, otherwise healthy
- Medications: Oral contraceptive pills
- Family history: Her mother had a pulmonary embolism during her second pregnancy. Her grandmother had died suddenly at the age of 45 of an unknown cause.
- Allergies: NKDA
- Social history: She is not sexually active. She smokes 1 pack cigarettes/week, and drinks 2-3 drinks a night on most weekends.
Questions:
- What is your working diagnosis based on the history?
- The clinical presentation of this female is highly suggestive of a pulmonary embolism, likely secondary to a DVT.
- What diagnostic imaging would be done on this female?
- Chest x-ray
- Duplex ultrasound imaging
- Radionuclide lung scan (V-Q scan)
- What labs would be drawn on this patient?
- CBC, platelet count, ABG, aPTT, PT/INR
- D-Dimer assay
- A genetic coagulopathy is suggested because of the age of the patient, as well as her family history. Testing for factor V leiden, protein C and S deficiency, antithrombin III and anti-phospholipid antibodies may be helpful in the diagnosis of her condition.
- What are risk factors for DVT in this patient?
- Family history
- Smoking
- Oral contraceptive pills