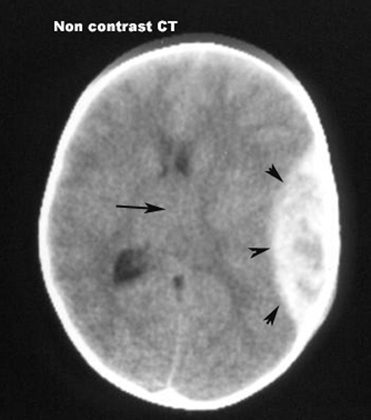
Epidural Hematoma
- Arrowheads point to the epidural hematoma, which is a collection of blood between the skull and the dura.
- It typically has a biconvex margin towards the brain surface.
- Arrow points to shift of midline to the right.
 |
Epidural Hematoma
|
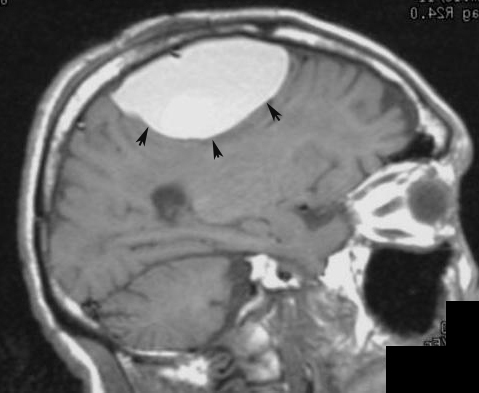 |
Epidural Hematoma / MRI |
Defined as bleeding between the inner region of the skull and the dura mater, they are most commonly associated with head trauma.
Defined as bleeding between the dura and the arachnoid mater, they are usually caused by movement of the brain relative to the skull—as in acceleration-deceleration type injuries—resulting in injury to an artery or vein within or over the brain surface. Subdural hematoma is located between the layers of dura and arachnoid mater, covering the cerebral hemispheres whereas intracerebral hematoma is localized within the brain substance. Acute subdural hematoma is recognized by CT as an area of peripheral zone of crescentic shaped increased density, outside the surface of the brain (arrows). Most subdural hematoma is caused by tear of bridging cortical veins. Acute subdural hematoma can evolve over a period of time and can thus be classified as acute, subacute and chronic hematoma.
Acute subdural hematoma (up to 7 days old): High CT density (40-90HU).
Subacute Subdural Hematoma (7 to 21 days old): The CT density of acute blood gradually decreases and becomes isodense with adjacent brain, thus less readily visible and can be easily overlooked.
Chronic subdural hematoma : Chronic (over 21 days old): Acute blood as it evolves, it undergoes liquefaction, and also mixes with cerebrospinal fluid from adjacent subarachnoid space, thus converting into a serosanguineous fluid. This fluid has low CT density reaching close or similar to cerebrospinal fluid. Slow movement of subarachnoid fluid into the subdural hematoma can give rise to gradual expansion of subdural hematoma that can exert mass effect upon the adjacent brain with or without brain edema. This can produce herniation of the brain resulting in sudden decompensation of the patient leading to coma.
Thus even a chronic subdural hematoma might need an emergent neurosurgical intervention.